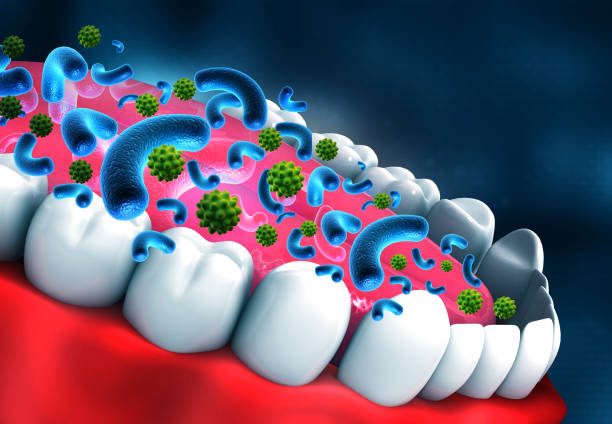
Oral yeast infections, also called oral thrush, happen when an overgrowth of the Candida fungus occurs in your mouth. This imbalance can occur for a multitude of reasons, typically associated with things such as compromised immune systems, long term use of antibiotics or certain health conditions. Many people hold false beliefs about yeast infections, thinking they are specific to the skin or sexual organs. But oral yeast infections are a very common occurrence, especially for some people.
An incorrect assumption is that a fungal infection in the mouth may only be caused by poor oral hygiene. Although care of the mouth is involved, in some cases, yeast infections cannot be avoided even when people practice good oral health. The patches form not because of dirt but because the body’s delicate equilibrium has been disturbed. For instance, oral yeast infections are also quite different than other types. In the mouth, it usually shows outwardly as white patches of skin on the tongue or inner cheeks and gums that you rarely see in other yeast-related infections.

In this situation, being able to spot the symptoms of an oral yeast infection will be extremely useful in allowing you act quickly on a potential treatment. Some symptoms to look for are a thick white coating in the mouth, difficulty swallowing and redness or soreness where it is located. Remember that symptoms may be more severe in babies, the elderly and people with weaker immune systems. People with weakened immune systems (including those on chemotherapy or living with HIV) could also have more prolonged infections that need specific treatments. If you observe visual cues of white lesions that come off as cottage cheese then it is a strong sign but still refer to a healthcare provider for a better understanding.
Causes and Risk Factors: When Yeast Becomes a Problem Calling For Doctor’s Advice

Candida is a kind of fungus that naturally exists in your mouth and other parts of your body. If in small quantities, it is usually harmless but an imbalance can cause yeast to grow quickly making the real problem called oral candidiasis. Multiple factors can throw off the good bacteria and Candida balance. For instance, taking antibiotics can wipe out friendly bacteria that keep Candida in check. The other major factors that create this imbalance is due to a modern lifestyle of stress, poor diet and weak immune system which also makes the human mouth an ideal environment for overgrowth.
Some people are more at risk of developing the infection than others. In fact, diabetes and other systemic diseases can increase the growth of candida in your mouth; because people with these conditions have more sugar in their saliva. People with dentures and those who have dry mouth conditions may also suffer more often. Anyone going through things like chemo and radiation treatments, as well anyone with conditions that weaken their immune system – like having the HIV virus – are particularly at risk. There are also two special cases: infants and the elderly, as they both have lower immune responses which makes it easier for yeast to thrive within their mouth.
If you suspect that you have an oral yeast infection, it is important to pay a visit to your doctor. A doctor can diagnose it for you and suggest the right treatment, maybe antifungal mouthwash or tablets or just some tips of life in general to follow. Depending on how severe your condition is, dentists and general practitioners may work together with infectious disease specialists or dermatologists to diagnose your symptoms. The consultation is likely to include questions about your medical history, any symptoms you have been experiencing, and recent medication use. Your doctor may do a visual exam of your mouth and look for lesions or sores that contain the Candida fungus, then get a sample from them via swab to be tested at a lab.
Treatment Options: From Medication to Home Remedies

More often, antifungal medications are used to treat oral yeast infections. These include nystatin and fluconazole, which are both medication to treat yeast infections by combatting the overgrowth of Candida in your mouth. Based on the severity of the infection, they can be a mouth wash or lozenges or oral tablets. Take the full amount of medication just as prescribed even if your symptoms quickly subside because stopping medication too early can leave some of the bad bacteria alive which would then cause a recurrence.
On top of that, many people seek non-medicinal means to help with their recovery. Rinsing your mouth with salty water or diluted hydrogen peroxide may relieve symptoms, but this is not a substitute for antifungal treatment. Eating foods containing probiotics can also help to support the health of good bacteria in your mouth. Nevertheless, please remember that these are home remedies & perhaps cannot work individually to wipe out the infection. Powerful nutrients in the immune diet can help with both treatment and prevention of yeast infections, so maintaining a low sugar / no junk food diet is also important.
Delaying treatment for oral yeast infections can lead to a variety of problems. If you neglect treatment, the infection can spread to other areas of the body, especially in immuno-compromised people. Moreover, continued pain, trouble eating or swallowing of food and a consistent taste of something bad in the mouth can cause havoc with daily life. When left untreated, oral yeast infections can develop into chronic conditions that are much harder to treat and may lead to a negative impact on your overall oral as well as general health. Therefore, I much recommend that treatment should be immediate to prevent these complications and address the infection at its early stage.
Prevention Strategies: Keeping Yeast Infections at Bay

The most effective way to avoid fungal (yeast) infections in the mouth is through good daily oral hygiene. Brushing, flossing and using an oral rinse, this will help eliminate and remove any food particles or bacteria that could be acting as a tasty treat to fuel the overgrowth of Candida. An extra care should be taken by denture wearers in cleaning and disinfecting them every day; people with the greatest risk of exposure; health workers, for instance might have personal dental tools they use only at work. Simple practices such as drinking enough water and avoiding sugary foods can also help prevent sugar from being consumed that will facilitate the growth of Candida.
Another major consideration is diet. Candida feeds off of sugar, so simply cutting down on sweets and processed foods (as well as some starchy carbohydrates) can help starve the Candida fungus.
Use probiotics: Containing good bacteria, (like those in yogurt or kefir), these can help support healthy levels of the beneficial Candida-fighting bugs living in your gut.
Consume enough fiber, vitamins and antioxidants all act as immune boosters layering defenses so it is hard for infections to take hold. In some cases, particularly those with weakened immune systems due to medications or a disease state, healthcare providers may suggest prophylactic antifungal therapy in order to prevent these infections from occurring.
Living with a yeast infection in your mouth can be emotionally exhausting. For those who suffer from frequent infections, it can be embarrassing to deal with symptoms like bad breath and white covering on the tongue. The typical coping strategies of those who have been through this can be boiled down to being proactive, doing everything in your power after treatment has been prescribed good oral hygiene and a diet that lowers risk. Having help from both doctors and friends / family can be very important in managing the physical aspect, as well as LETTING YOURSELF FEEL ALL THE EMOTIONS that come your way. Talking this over with professionals can help them chart effective personalized healing plans, and discussing it with people who have experienced the same thing also provides a solid validation as well as tips on how to get by.
Thank you for reading my article about “Can You Get Yeast Infection In Your Mouth?” and I would love to receive your comments down below, in case of any.